AI-Driven Decision Support in Vision Care
The field of vision care is undergoing transformation and has been better supplemented through artificial intelligence to enhance the effectiveness of diagnostics, patient outcomes, and support in clinical decision-making. AI-based diagnostic and decision-support systems have proven to have high accuracy in detecting, classifying, and even predicting ocular diseases using advanced algorithms, deep learning, and big data analytics. Such systems assist eye care professionals with identifying diseases like diabetic retinopathy, glaucoma, age-related macular degeneration (AMD), and refractive errors.
Role of AI in Vision Care
The significant aspects of artificial intelligence in vision care are as follows:
- Automated Screening and Early Diagnosis: AI algorithms could analyze retinal images, OCT scans, and other diagnostic data in real-time for possible signs of eye disease. This early intervention could prevent vision loss.
- Clinical Decision Support: Decision Support Systems (DSS) that include AI can provide ophthalmologists and optometrists with data, risk stratifications, and treatment options based on a patient’s information.
- Increased Accuracy & Automation: In other words, AI can reflect diagnostic errors by batching and cross-referencing datasets faster and more accurately than we can inform a physician.
- Tele-ophthalmology and Remote Access: AI could use screening and diagnostic technologies remotely to help reduce the number of digitally undiagnosed individuals and decongest our healthcare systems and services.
- Personalized Treatment Models: AI assesses treatment algorithms based on an individual patient profile that enhances medication adherence and care experience.
AI-based Eye Disease Diagnosis Process
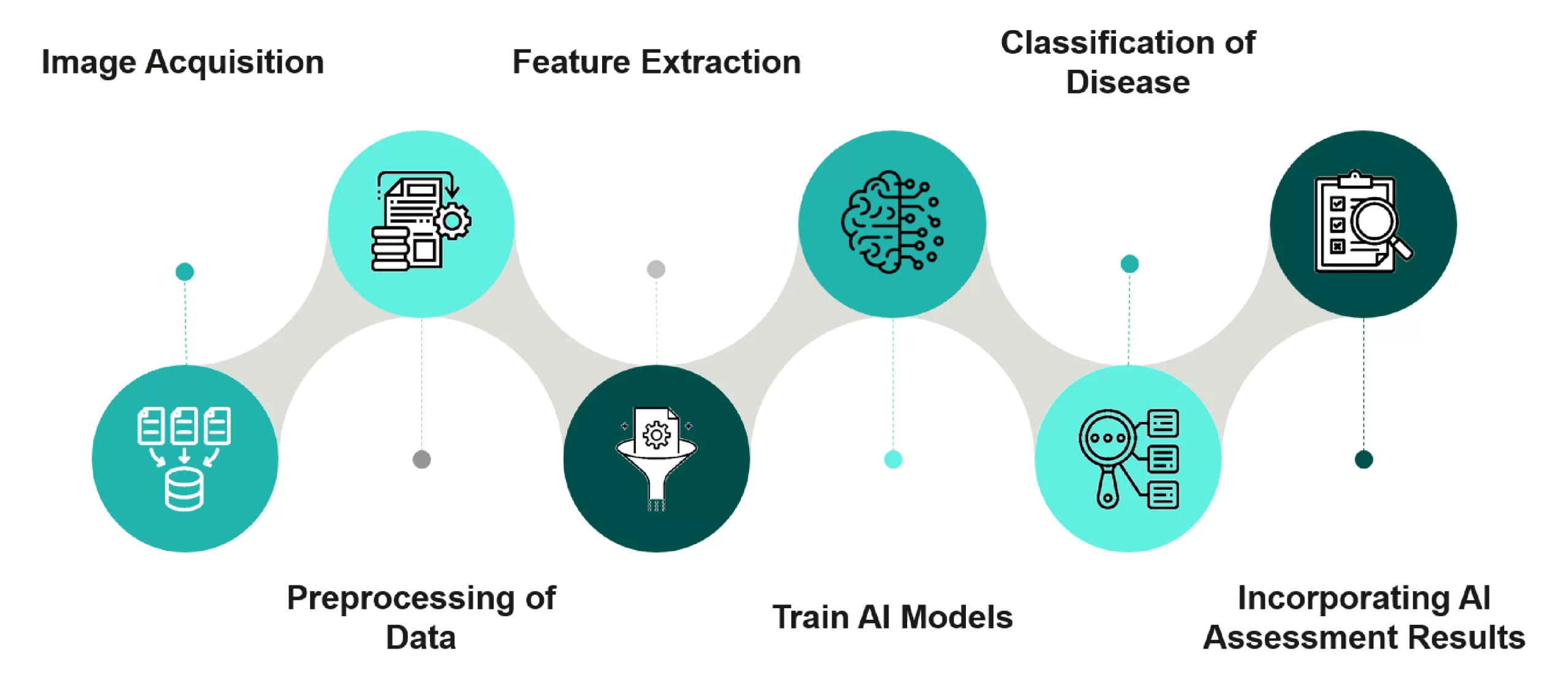
Figure 1: Process of AI-based Eye Disease Diagnosis
- Image Acquisition: The initial step is to capture images at the micro-dimension level using special equipment or instruments from the patient’s eye. These could be retinal scans, OCT images, or fundus photos.
- Preprocessing of Data: The preprocessing is done on the raw image data so as to improve image quality and standardize formats. Normalization and noise removal methods help bring the images into better clarity.
- Feature Extraction: The AI algorithms pre-process the data of the most pertinent images to extract features. These features can include optic disc morphology, vascular patterns, or lesions.
- Train AI Models: The trained features are used to develop a deep neural network (CNN) or any other AI model. The model is trained using labeled datasets to teach it as many disease patterns and classes as the labeled datasets support.
- Disease Classification: The AI algorithms will classify images into disease-specific categories (e.g., diabetic retinopathy, glaucoma, macular degeneration). Algorithms will use the patterns and features learned during training to classify the disease.
- Including AI Assessment Results: The AI assessment results will be included in the clinical process. As part of the process, ophthalmologists will compare a verified AI report with other standard diagnostic methods to monitor patient care effectively.
Benefits of AI-Powered Screening
AI has several benefits over traditional methods, such as:

Figure 2: Benefits of AI-Powered Screening
- Enhances Eye Care Access: Teleophthalmology using AI allows distant eye screening and diagnoses in regions where vulnerable people will never get access.
- Supports the Decision-Making of Clinicians: Decision support systems with AI as a back end assist ophthalmologists and optometrists.
- Early and Accurate Disease Detection: AI algorithms read retinal images and other aspects of diagnostic data to identify markers of certain eye pathologies.
- Tailored Treatment: AI customizes the interventions for each patient based on their profile, which can increase the effectiveness of a therapy.
- Economic Healthcare: Requires less use of expensive, high-risk procedures and unnecessary physician visits.
- Continuous Learning & Improvement: AI algorithms learn from each new set of data, which will help improve diagnostic performance over time.
- Avoid Preventable Blindness or Vision Impairment: AI can prevent unnecessary blindness by improving early detection and initiating timely treatment.
- Utilization of Wearable and Smartphone Technology: Artificially intelligent tools amalgamated into mobile devices enable self-assessment and prompt identification in the comfort of home.
Improvement Areas
Some of the key areas where improvement needs to be addressed include:
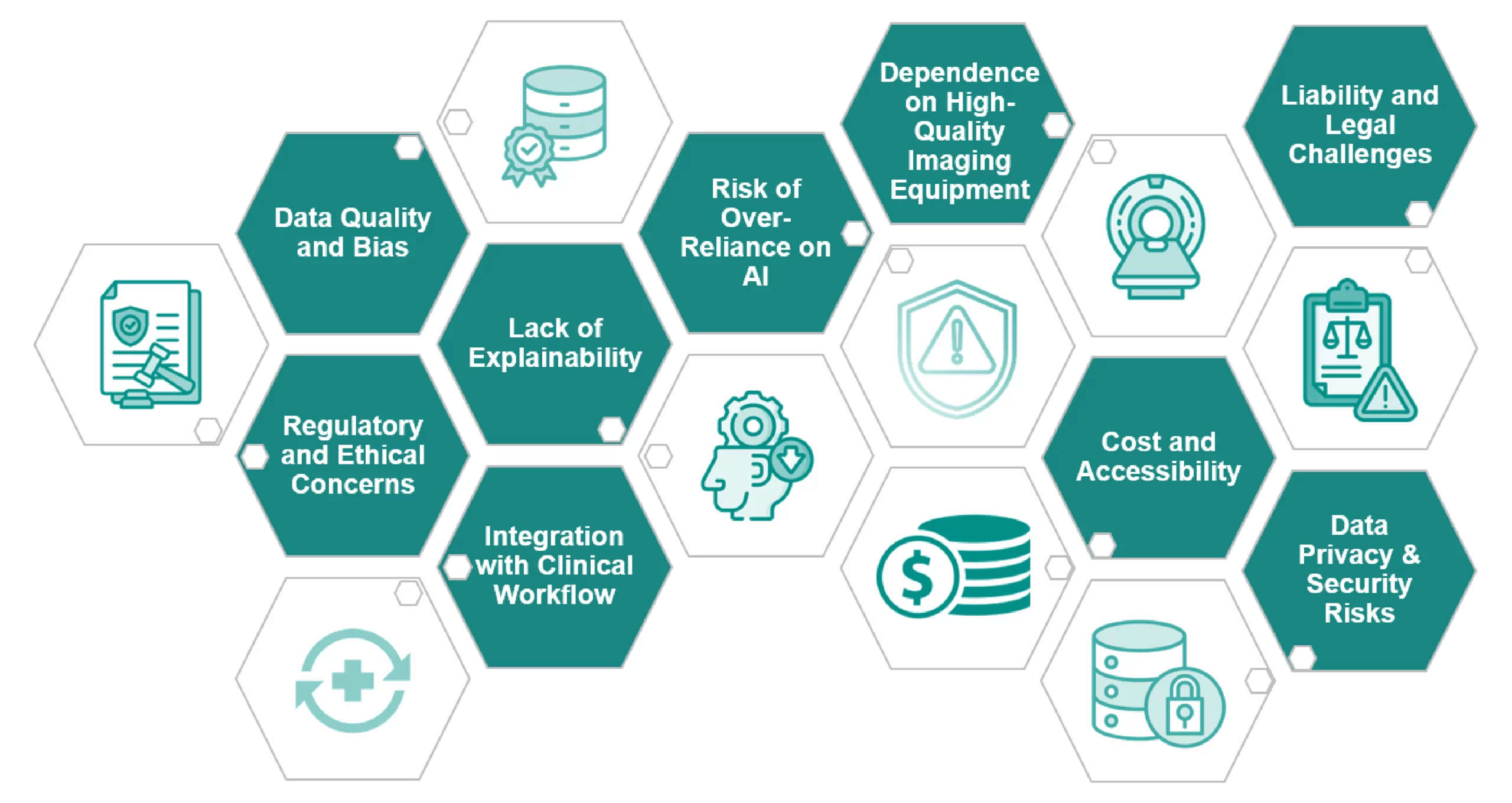
Figure 3: Improvement Areas
- Data Quality and Bias: AI systems are trained on massive datasets, but if the datasets are incomplete, imbalanced, or biased, then the resulting models will not be equally accurate across populations. Diverse datasets are essential, as their absence may lead to discrepancies in diagnosis.
- Regulatory and Ethical Concerns: AI-powered diagnostic tools need to meet firm healthcare regulations (e.g., FDA, CE marking) prior to clinical application. Ethical issues surrounding AI decision-making, patient data privacy, and accountability have not been addressed yet.
- Lack of Explainability: The majority of AI models are “black boxes,” i.e., their decision process is not transparent, and clinicians cannot interpret the flow of logic.
- Integration with Clinical Workflow: AI applications must be embedded directly within present-day healthcare IT and EMR. Workflow mess and practitioner pushback will prevent adoption.
- Dependence on High-Quality Imaging Equipment: AI precision is reliant on high-resolution retinal images and other diagnostic information that may not always be accessible across all locations, particularly in resource-poor areas. Image quality variability among various devices may affect AI.
- Risk of Over-Reliance on AI: Heavy use of AI translates to lost clinical reasoning and decision-making skills for physicians.
- Cost & Accessibility: Excessive development and implementation expenses might restrict the accessibility of AI-based diagnostic tools in resource-poor environments.
- Liability & Legal Challenges: When an AI system provides an erroneous diagnosis and causes harm, it becomes difficult to ascertain liability among the AI developer, healthcare professional, and hospital.
- Data Privacy & Security Risks: Vision care AI relies on highly sensitive patient data, and there are still risks of data misuse and cyberattacks. Data regulations must ensure privacy and confidentiality, making an AI rollout more complex.
Market Dynamics
The market dynamics of AI-based ophthalmic diagnostics include the following drivers, opportunities, and challenges:
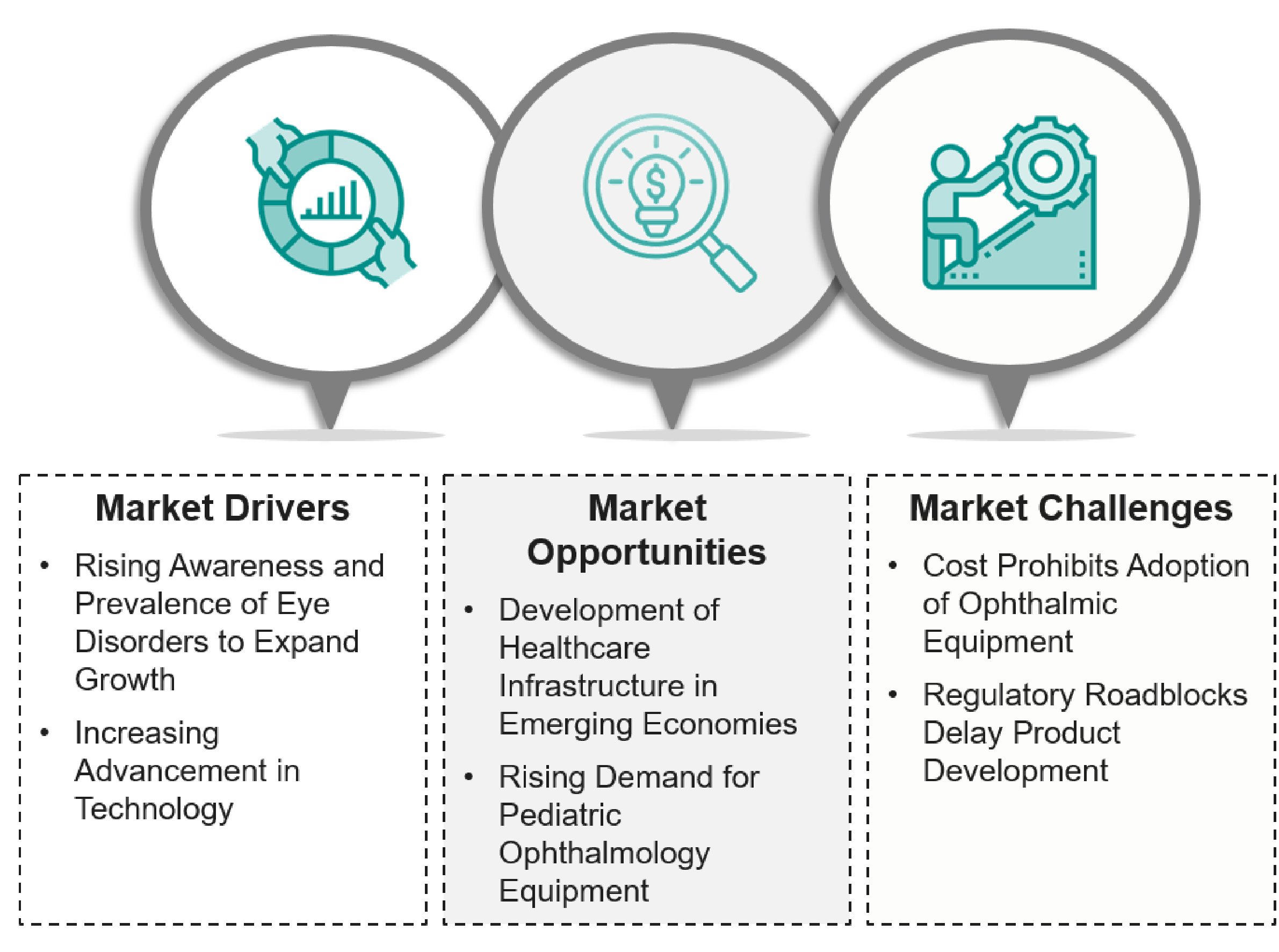
Figure 4: Market Dynamics of AI-based Ophthalmic Diagnostics
Market Drivers
- Rising Awareness and Prevalence of Eye Disorders to Expand Growth: There is an increasing awareness of eye diseases worldwide, and the availability of eye care is improving along with government initiatives.
- Increasing Advancement in Technology: Healthcare professionals’ access to the newest technology, such as OCT with AI, is expected to enhance the ease of use for subsequent adoption of the tools.
Market Opportunities
- Development of Healthcare Infrastructure in Emerging Economies: Emerging economies represent a different set of opportunities through healthcare infrastructure development, increasing middle-class population, low-cost equipment, and medical tourism.
- Rising Demand for Pediatric Ophthalmology Equipment: There is increasing demand for pediatric ophthalmology because of more emphasis on children’s eye health and advances in devices designed to care for children. There are also more cases of children who are developing ocular disorders, and when you are trying to diagnose ocular disorders, there is a lot of urgency that is driving demand for equipment.
Market Challenges
- Cost Prohibits Adoption of Ophthalmic Equipment: Additional lower-cost options are preferred, since the steep cost of ophthalmic diagnostic equipment represents the biggest barrier to adoption.
- Regulatory Roadblocks Delay Product Development: Regulatory considerations are typically stringent and can block firms’ growth. In particular, regulatory amendments or delays can result in an extension of time to market, contaminating effective product realization. The approval process can cost a lot and reappear constantly, which greatly interferes with the firm’s ability to iterate quickly and capture competitive advantage.
Latest Advancements in AI-Powered Diagnostics in Vision Care
AI is revolutionizing eye care with its ability to diagnose, treat, and care for patients. The following are some advancements in AI-powered diagnostics in vision care:
- AI-Powered Kiosks (Eyebot): They offer a service of automated, self-serve vision tests via AI-driven terminal kiosks that complete the necessary testing in only 90 seconds, also providing instant prescriptions for eyeglasses.
- Radius 1.0 Software (Radius XR): An updated version of the software for perimetric exams that incorporates a range of new options to enhance diagnostic capabilities for glaucoma management. The Radius is a portable system that combines medical-grade diagnostics with business management and patient education.
- EyeArt AI Eye Screening System (Eyenuk): This is the most rigorously validated AI technology for the autonomous detection of diabetic retinopathy. It enables point-of-care, real-time diabetic retinopathy screening in primary care practices, diabetes centers, and optometric offices, enabling physicians, including non-ophthalmologists, to promptly and accurately identify referable DR patients during a diabetic patient’s routine examination.
Key Players in AI-Powered Diagnostics in Vision Care
Key players working in AI-powered diagnostics and decision support systems in vision care include:

Figure 5: Key Players in AI-Powered Diagnostics in Vision Care
Future of AI in Vision Care
As technology develops and AI continues to progress, AI’s involvement in wearable technology, smartphone-based diagnoses, and robotic surgery could boost vision care. AI models may also help predict the progression of disease and facilitate the appropriate treatment plan.
The future of eye care will be more accurate, effective, and easily obtained by using AI coupled with conventional eye care knowledge to care for our patients.
Conclusion
AI-powered diagnostics and decision support are redefining vision care for early detection at scale, accurate diagnosis, and tailored treatment. In the real world, AI makes the scale of detection and precision driven by data available for accuracy in both conditions. AI is closing gaps in remote monitoring and deep learning through teleophthalmology and automated screening, especially in emerging markets, to bridge the expertise vs accessibility gap. With the increase in adoption, AI offerings will be crucial in reducing blindness due to avoidable conditions and enhancing the general health of the eyes worldwide.
Let's Take the Conversation Forward
Reach out to Stellarix experts for tailored solutions to streamline your operations and achieve
measurable business excellence.