Precision medicine, sometimes known as personalized medicine, is a way healthcare providers can offer and plan specific patient care based on the particular genes, proteins, and other substances in a person’s body. This is largely based on knowing the effects of changes in specific genes (and proteins) inside cells. In precision medicine, doctors use information from lab tests to put together a plan of care that usually includes specific recommendations.
Diagnostic testing is frequently used in precision medicine to determine appropriate and optimal therapeutics based on a patient’s genetic content or other molecular/cellular studies. It can also be used to develop one-of-a-kind medicinal products for specific individuals, such as patient-specific tissue or organs that can be used to adapt therapies for different patients. Precision medicine tools include molecular diagnostics, imaging, and analytics.
Introduction to Precision Medicine
Every person has a unique variation of the human genome. Genes are pieces of DNA inside each cell. They tell the cell how to make the proteins it needs to function. Each gene contains the code to make a certain protein, and each protein has a specific job in the cell. During cell division, the genes inside the cell are copied. A gene change happens when a mistake in the copying process occurs. Some gene changes can be harmful, while others may not cause any problems.
Precision medicine means looking at how changes in specific genes or proteins in a person’s cells might affect their care, such as their treatment options. Precision medicine is a medical model that proposes the customization of healthcare, with medical decisions, treatments, practices, or products being tailored to a subgroup of patients instead of a one-drug-fits-all model. Even though genetics and genomics are well-established fields in developed nations, developing nations have made significant strides in precision medicine and genetics over the past ten years in terms of legislation, product approvals, and the application of cutting-edge techniques and procedures in healthcare.
How Does Precision Medicine Differ From Personalized Medicine?
The National Research Council (NRC) has expressed concern that the term “personalized medicine” could be misunderstood to imply that every patient can receive a completely unique treatment plan, which is untrue. According to the NRC, precision medicine is the practice of customizing medical care to each patient’s unique needs. It refers to the capacity to divide people into subpopulations that vary in how they react to a given treatment or by how susceptible they are to a certain disease. However, it is not the actual process of creating medications or medical devices that are specific to a patient. While this idea is also expressed by the term “personalized medicine,” it is occasionally misconstrued to suggest that each patient can have a customized course of therapy.
Pharmacogenomics, Pharmacogenetics and Pharmacodiagnostics in Precision Medicine
The therapeutic science of pharmacogenomics assists in determining the genes that influence a patient’s response to a medication. It provides knowledge on genes that impact an individual’s susceptibility to a specific illness. The correlation of DNA mutations with pharmacokinetic, pharmacodynamic, and immunogenic endpoints promotes research on the consequences of acquired and inherited genetic variation on patient response to medication.
Pharmacogenetic testing is widely used for medications for cancer and blood coagulation. By using pharmacogenetics and pharmacogenomics, the varied drug responses in each patient and linked to their genetic profile. Hence, personalized medicines are being developed for diseases like cancer, neurological disorders, autoimmune diseases, and gynecological disorders. Pharmacodiagnostics or Theranostics is a branch of medicine that combines molecular diagnostic tests with specified targeted therapy. It helps in estimating the safety and toxicity of targeted nuclear therapies. It involves coupling diagnostic imaging and therapy using the same or similar molecules administered in different doses or radiolabeled differently.
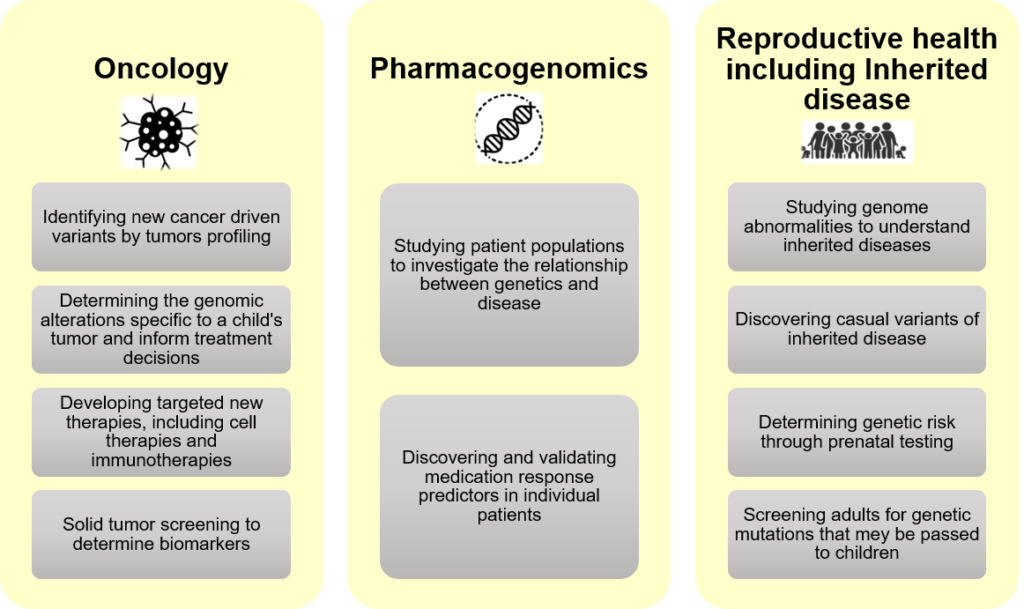
Figure 1: Applications of Precision Medicine
Precision medicine helps better diagnose with early intervention, more efficient drug development, and targeted therapies. It has been adopted across various fields. Most importantly in cancer research and inherited diseases, for diagnosis and treatment using next-generation sequencing (NGS) technology. A wide range of examples of precision medicine applications are mentioned in the figure above:
Precision Medicine: Challenges
- The initial costs of drug development are high due to the complexity of many analytic and diagnostic procedures involved wherein an exclusive patient population is selected.
- Finding and targeting the correct intermediate molecule causing the disease is also difficult.
- Incorrect laboratory testing can leave the treatment ineffective or toxic, as unnecessary administration may cause toxicity or other adverse events.
- Ethical issues also raise concerns, as many government and university bodies have yet to develop stern standards for diagnosing genetic disorders before prescribing personalized medicines. The anonymization of data and its security are also big issues.
Current Market Overview
Biotechnology has advanced tremendously in the last decade, and the incorporation of AI in healthcare is helping to expand the market size. The global oncology precision medicine can grow at CAGR 11.2 until 2030. The Asia Pacific region may have the largest CAGR. The non-oncology precision medicine size may increase up to 130 billion dollars by 2030
Key Players in the Domain
Many companies are working towards the growth of the precision medicine market globally.
In February 2023, Roche received EC approval for expansion of the Hemlibra (emicizumab) European Union (EU) marketing authorization based on the HAVEN 6 results
- In January 2022, AstraZeneca collaborated with Scorpion Therapeutics to develop and commercialize precision medicine against hard-to-target cancer proteins
- With the launch of a data-driven precision medicine initiative in May 2021, AdventHealth and Sema4 expanded its genomics program. This initiative organized and integrated longitudinal patient data with molecular testing data
- A few other players working in this domain are Novartis, Pfizer, Catalent, Johnson & Johnson, Roche, Sanofi, Bristol Myers Squibb, Amgen, etc.
Precision Medicine Startups
Early-stage companies and start-ups have advanced precision medicine by applying Artificial Intelligence (AI)/Deep Learning, clinical genomics, and other latest technologies.
Table 1: Precision Medicine Startups

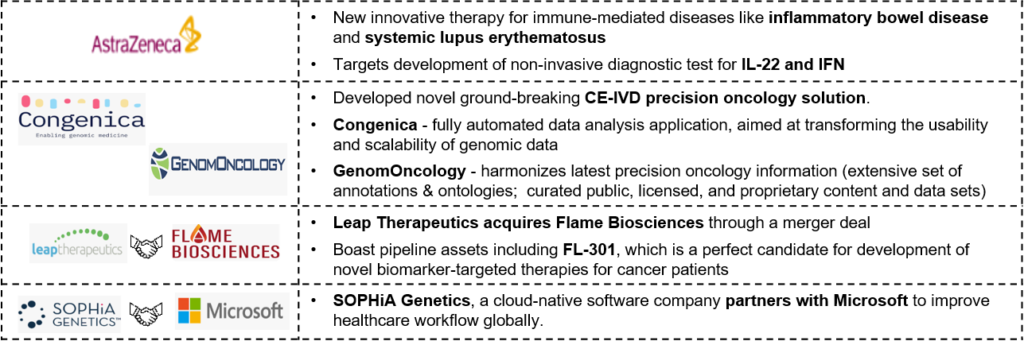
Recent News Around Precision Medicine
The precision medicine industry is already moving to maximize the potential of cutting-edge technology, such as digital solutions, AI-enabled products, etc. Moreover, the field is gaining tremendous traction and will become more and more significant in healthcare delivery in the future
Table 2: Recent News Around Precision Medicine
Conclusion
Combining the human DNA, environmental variables, illness evaluations, and medicines to achieve better therapeutic outcomes is the primary goal of precision medicine. The development of personalized medicine involves not only scientists, academia, and industry players but also patients. Patient satisfaction comes with effective disease management and improved quality of life. Also, important information related to treatment strategy should be shared with them to build patient trust and treatment compliance. Conventional medicine continues to hold a prominent place in treatment and disease management. However, precision medicine shows a promising future in providing the “right treatment to the right patient at the right time”.