Home-Healthcare and Technology: Transforming Patient Care
Home healthcare or Hospital-at-home (HAH) is a futuristic, sustainable, and cutting-edge approach to healthcare. Healthcare management can benefit from this model’s cost and quality improvement; for physicians, offering patient-centered medical care and avoiding hospitalization and complications is beneficial. The home-based model of care is an acute critical care model for patients at their homes and helps them prevent hospitalizations and the complications that arise with them. This care is typically provided to older patients with chronic illnesses and multiple other health conditions.
This transition to home care is now happening at an unprecedented rate because of newer evidence that supports delivering care at home, improvement in efficiency and satisfaction, lower cost, and newer technological innovations digitized in recent years along with the pandemic.
Emerging Technologies Facilitating a Transition to Home Care
Home healthcare has emerged as one of the fastest-growing segments in the healthcare industry, which has significantly boosted with the onset of the pandemic; some of the subsectors in this segment include hospice, home 24/7 nursing care, home medical equipment supply delivery, and at-home diagnostics. The focus is gradually shifting to the ease of implementation of technological solutions to reduce the barriers and difficulties of the home healthcare industry.
Some solutions are being launched by start-ups with the help of which they are offering remote patient monitoring and telehealth services, smart home automation solutions, assistive robotic technologies, applications based on artificial intelligence and machine learning, and virtual reality therapy solutions. The trends that shape the future of home care solutions empowering patients, their families, and care providers to achieve comprehensive care at home are as follows:
1. Remote Patient Monitoring
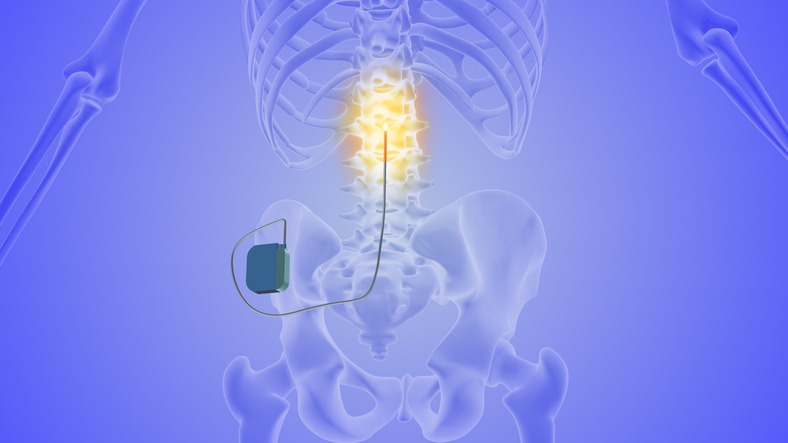
Remote Patient Monitoring (RPM) remains a key reason for transforming home care since it enables healthcare providers to monitor their patient’s condition from a distance. It eradicates and reduces factors like restricted access to care, geographical restrictions, and limited hospitalization admissions. Some current advances used in the RPM system include tracking invasive medical devices, smart sensors, and telemedicine applications, among others. Home care technologies enrich patient involvement, early disease detection, individualized management strategies, and prompt actions.
2. Virtual Reality (VR) Therapy
The application of VR is expected to bring numerous advantages for elderly people—for instance, a concept of generally healthy aging that includes health-based games, social connectivity through digital interfaces, therapy, and assistance to navigate day-to-day life. Advancements in technologies such as robotic devices and VR headsets help control stroke patients’ neurorehabilitation, allowing them to begin the recovery process faster and providing them with properly guided exercises. These technologies enhance home care by offering individualized approaches, enhancing consumers’ interactions and participation, and facilitating teletherapy.
3. Smart Home Solutions
Smart home solutions have been developed through the latest developments to enable better and improved patient care. Some of the examples are voice-activated home devices, IoT-connected appliances, and movement-tracking gadgets. Some benefits include ease of use, availability of up-to-date information, and preventive health care. Smart Home Solutions bring down costs, optimize resource use, and enhance staff well-being for healthcare workers.
4. Wearable Technology
Wearable devices are proving to be highly useful in remote patient monitoring to enable timely health checks and mitigate complications. Wearable technology has become popular and has played a role in changing how healthcare is provided. Fitbits, smartwatches, and wearable monitors are some of the examples that create real-time data collection and individualized possibilities.

Figure 1: Home Healthcare Industry Trends and Promising Start-ups
5. Assistive Robotics
The use of assistive robots in in-home care reduces cases of insufficient caregivers and tackles social isolation due to loneliness. These include the Socially Assistive Robots (SARs), robotic companions, nursing robots, and sanitation robots. They advance home care through patients’ involvement, friendly presence, and the ability to perform tasks. Robots bring availability, better services, and less burden and stress to care service staff members.
6. AI-powered Personalized Care
Home care is built around a mountain of quotidian tasks invasive to the support worker’s attention and concentration. Thus, there is a demand for new AI personalized solutions, including chatbots, predictive analysis, and NLP models. Technological advancements in AI are helping home care facilities avoid performing routine operations, giving caregivers a clear view of real-time analysis of their patients and making smart decisions for better results.
7. mHealth
Mobility and accessibility are two of the most fundamental requirements for properly managing the patient’s health at home. mHealth responds to challenges by leveraging simple mobile application solutions and chronic disease-specific mobile application solutions. Healthcare stakeholders use mHealth solutions to reduce expenditure and enjoy better mobility when operating home care solutions.
8. Cloud-Based Platform/Workflow
Several software modules’ upgrades and continuous development require integration within one platform. Hence, cloud platforms are obligatory for in-home care for such purposes because of their impressive data processing capabilities and the cooperation of interacting stakeholders in real-time. Such applications allow secure data exchange and navigation, which helps avoid information isolation and allows obtaining useful data both for patients and providers.
9. Electronic Health Record Systems
EHRs are real-time patient health records that offer complete, accurate, and up-to-date data at the time of treatment. They allow for coordinated care and safe information exchange and enhance the diagnostic processes. EHRs save costs for home care stakeholders by eliminating reduced contextualization, repetitive testing, and decisions based on patient files.
10. At-home Medication Systems
Smart boxes, pill dispensers, and other medication systems at home enhance home care since they offer efficient medication management services. They make sure the right drugs are administered to a person in the right quantity and at the right time to avoid complications. Compared to traditional methods, the systems mentioned above have several advantages, including modality alert, individualized medication regimen, and medication compliance.
AI and Automation in the Home HealthCare – A Game Changer
The shift to utilizing AI technology in in-home care is a positive change as it enhances not only the quality of the healthcare system but also the experiences of patients, agencies, providers, staff members, etc. In the long term, this multifaceted approach aims at better value-based care from independent practices, patient satisfaction, and better ways of managing health issues at home.
AI goes a step further and imbues automation with the capacity to make decisions such as identifying appropriate referrals or simply analyzing feedback received from the client. AI and automation have kicked in and dramatically enormously affected home care. Some examples of advantages are better client and caregiver experience, overall quality of caregiving, more accessibility and affordability, real-time synchronization and notifications, efficient workflow management, error tracking and reporting, and others.
Through automation, home healthcare providers can enable system interoperability, interface with other systems in real time, and manage several processes simultaneously. Automation makes work easier, reduces errors, and generally leads to better and more efficient patient treatment in home settings.

Figure 2: Applications of AI and Automation in Home Healthcare
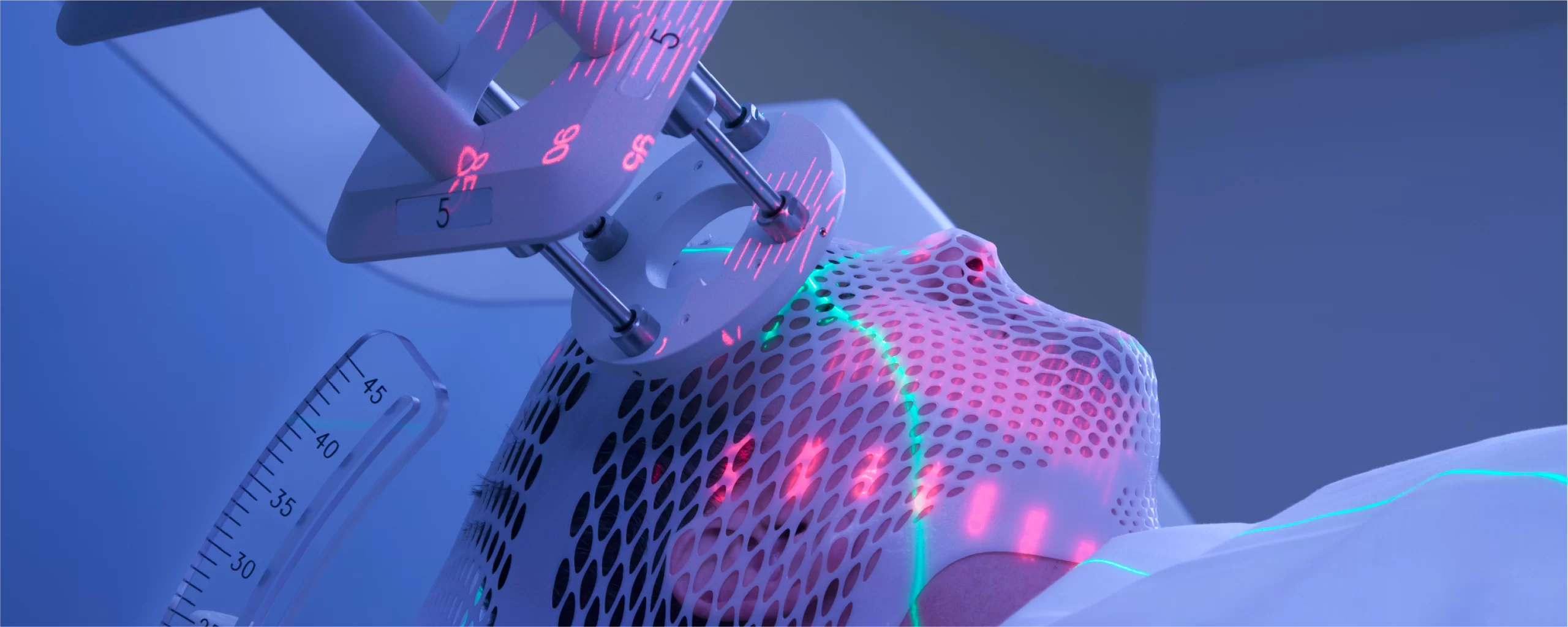
The Importance of Medical Device Technology for Home Care
Medical equipment has evolved to support the need in acute or palliative and critical care situations. For conditions like diabetes, hypertension, and the like that require constant checks, affordable and easy-to-use products such as glucose meters, blood pressure measuring tools, and so forth are widespread in several households. This bodes well for the elderly and those with chronic lifestyle diseases. Hence, an ideal home care device should be portable, require little effort/involvement to operate, be safe, enhance the quality of outcome, and be efficient financially in the short and long run.

Figure 3: Important Parameters for Home Healthcare Devices
Some devices can be used at home to address diabetes, pneumonia, emphysema, sleep apnea, open and/or closed wounds, renal failure, and infection. For instance, in the home care of high-risk cardiac patients, wearable smart watches for cardiac monitoring and wearable cardioverter defibrillators are being increasingly used to gradually discharge high-risk cardiovascular patients from the hospital.

Figure 4: Advanced At-home Medical Devices and Diagnostics
Challenges and Hurdles
Hospital-at-home, where patients receive the best care for diseases comparable to medical centers from doctors at home, eliminated many challenges during the pandemic. They have also been found useful in enhancing revenues and delivering medical solutions that are more effective in satisfying both patients and clinicians. This strategy of the hospital-at-home model has disadvantages and barriers, including problems with billing and reimbursement, conflict between doctors and patients, safety issues, and the near absence of research-based evidence on its efficacy, along with many technical and organizational issues that have to be resolved to support high-quality care delivery in patients’ homes.
Issues that must be addressed by organizations in derivative care delivery, specifically within the hospital-at-home or healthcare-at-home framework, are the following:
1. Financial or Reimbursement
The effectiveness and real ROI achieved from the hospital-at-home model have made various health organizations commit more resources to enhancing the quality of home care. However, specific issues pertain to the financial perspective when implementing such solutions.
Limited insurance hinders families from accessing care, especially long-term care, which Medicare does not fund.
2. Regulatory Complexity
Health care, in general, is sensitive and a well-guarded area; therefore, home-based care also operates under strict laws. An exceptional at-home program must address collaboration with CMS and audit organizations by getting approval and designating registration for patients and employees.
High expectations may lead to significant resources required to audit program quality and safety. Another area of substantial regulatory pressure is the privacy and security of patient information, consent, and documentation.
3. Staffing or Workforce Shortage
Another noticeable issue remains the problem of staff shortage, which, in turn, contributes to extended time for receiving assistance and, therefore, longer waits. Health care today is facing a big challenge of staffing shortages, where nurses are complaining of being burnt out with long hours and fatigue. Hospital-at-home has a positive impact on this in that it will enable the caregivers to have better flexibility and be exposed to working in different settings.
Healthcare providers require educating and enhancing the staff’s skills to fulfill patients’ requirements in in-home care facilities and learning about cases with high-intensity requirements and emergencies.
4. Clinical
Healthcare providers should establish admission criteria and protocols to distinguish between hospital-at-home and typical inpatient care settings.
When Hospital-at-Home is the planned course, the care provided at home shall not be lower than the quality of any inpatient setting for any diagnosis being contemplated for admission. To provide quality and indeed person-centered care within the home setting that is advantageous for the healing process, certain necessities need to be set, technology and services need to be integrated, and results must be assessed and monitored.
5. Social or Quality of Care and Client Satisfaction
Consistency of care becomes an issue due to staff shortages, which impacts the development of a relationship with the patients and the quality of the care being provided.
Community factors that may impact any hospital-at-home program include equitable access to healthcare irrespective of the patient’s background, checking the home environment to establish its fitness for delivering required care, and the safety risks to patients and staff. Integrating an at-home program should consider the patient perspective of quality care, quality standards across program sustainment, and all stakeholders’ safety.
6. Technological or Data Integration
Many home care providers continue to employ various software systems, which can create data compatibility problems when sharing information with other providers. Implementing new technologies and incorporating them into home care practices can pose a significant challenge to small agencies due to their rather scarce resource base.
There should be ample technology to complement the theme of home healthcare. Hospital-at-home operations will necessitate the use of remote and portable clinical devices, home broadband connectivity, and many others while adhering to compliance with security and regulatory requirements.

Figure 5: Challenges and Hurdles – Home Healthcare
Why Home Health Care Will Predominate in the Future
For several years, hospitals have remained the central facilities through which care delivery to patients, be it diagnostic or therapeutic, has been attracted. However, in a hospital setting, a few health workers attend to the group of patients, and the caregivers cannot spend adequate time with each patient to assess their needs and their response to the treatment administered to them, which affects their well-being. At the same time, the shortage of healthcare workers in some parts of the world is suffocating the healthcare system.
Moreover, in-hospital care entails the patient developing hospital-acquired infections that impliedly affect the patient’s well-being and consequently help raise the mortality rate. This precipitated the demand for home healthcare as it eradicates the key issues of hospital care, is more convenient to patients, enhances better health, and is cheaper for healthcare providers. Also, the at-home healthcare model is ideal with the expanding cases of aging people and chronic disease patients who need round-the-clock care.
Home healthcare makes the delivery of healthcare services decentralized, thus providing flexible and timely healthcare to all and completing the continuum of care. In this context, ambulatory patients can pursue daily activities more easily than recipients of in-hospital treatment, which consequently affects patients’ physiological status and life quality. Patients, especially the elderly ones and those with confined mobility, would instead be treated in the comfort of their homes.
Some studies reveal that home care for chronic disease patients decreases the mean unadjusted number of days of hospital stay, cost of care, and readmission rate compared to hospital-based care. Additionally, the 2020 pandemic and the successive intermittent COVID-19 waves have shifted patient preference towards home healthcare to reduce the likelihood of acquiring infections within hospitals.
Conclusion
Home healthcare supports care at homes for the elderly boomer generation and offers access and flexibility to Gen X and Millennials for health services. As the general population grows, there is an increasing need for home healthcare, and hence, there is a likely shift towards home care since this mode of care delivery is cheaper than inpatient hospitals and nursing homes. This new type of healthcare solution has been applauded for being essential. Without a doubt, it will expand its size even more when a combination of complex AI algorithms and advanced systems of healthcare data exchange are integrated.
Thus, it can be concluded that there is great potential for the development of home care in healthcare markets, primarily due to various factors such as higher availability and accessibility of technologies, population aging, and the need for personalized and convenient services.
Further, to transition from a hospital environment to a home environment, hospitals are developing home healthcare programs for patient care at home. The business model also positions the healthcare provider where they can monitor the care being offered to the patients. In contrast, the complex business and supply chain issues are managed by the clinical enterprise company, which reduces the burden on the provider while enhancing the quality of care offered to patients.