Digital Framework of Digital Health Devices
Digital health has been on a rapid rise since the COVID-19 pandemic. Wearable health technology and non-wearable device-based solutions dominate the digital health market. Companies trying to penetrate this segment should understand the layout or conceptualize digital framework while designing solutions. This article provides an outlook on components of the digital framework, those digital frameworks utilized in producing digital health devices (wearables and non-wearables), and mobile health apps (m-health apps), highlighting variables driving faster adoption of technology.
Components of Digital Framework
The Digital Framework for designing and implementing wearables, non-wearables, and m-health apps includes multiple components. The components, i.e., devices and applications, operate in unison to provide real-time analysis to the consumer.
The four main components of the digital framework include the consumer, technology provider, devices & sensors, and application interface.
Wearable devices that are design-forward, innovative, and user-friendly are ideal for any new entrant to target the blue ocean of digital health-based solutions. To tap this blue ocean, the right digital framework provides a scaffolding to guide an organization.
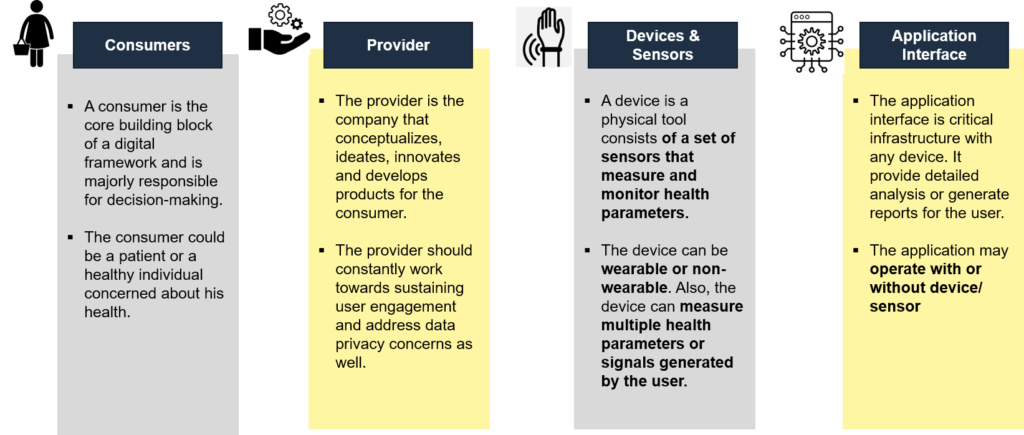
Figure 1: Components of Digital Framework
Information Quality Framework (IQFs) for Digital Health Technologies
- HIMSS Digital Health Framework: This framework utilizes digital health technology to assist healthcare organizations in transforming their operations and enhancing patient outcomes. Person-enabled health, workforce and governance, interoperability, predictive analytics, and digital health indicators are some of its components.
- Evidence Defined Framework: Developed to suit the demands of stakeholder groups, such as payers, health systems, trade organizations, and others, this framework evaluates the evidence supporting digital health interventions (DHIs). It has evidence-to-recommendation guidelines that identify adoption degrees that may be appropriate for a range of evidence-quality levels, a checklist that summarizes high-priority evidence considerations in digital health, and a Quick Start Guide that may help simplify DHI assessment.
- Digital Health Equity Framework: Designed to support the work of digital health tool designers in industry, health systems operations, and academics, this framework outlines important digital determinants of health (DDoH). It addresses the significance of a multi-level, root cause approach, looks at DDoHs at the individual, interpersonal, communal, and societal levels, and provides a useful case study that uses the framework.
- ORCHA Digital Health Assessment Framework: This framework has been specifically developed to evaluate digital health technologies, such as mobile apps and web-based tools utilized by both healthcare providers and consumers. It incorporates cutting-edge business intelligence technology combined with a team of experts who thoroughly assess each product.
Design, Evaluation Framework, and Life Cycle Models for Digital Health Interventions (DHIs)
The goal of the Design and Evaluation Framework for Digital Health Interventions (DEDHI framework) is to assist researchers and practitioners in moving from early conceptual DHI models to robust DHI implementations in the healthcare industry. It summarizes the implementation hurdles and assessment criteria that should be considered at each stage of the DHI life cycle.
Different phases of the DEDHI framework are:
- Preparation Phase: To define a DHI’s conceptual and technological foundation
- Optimization Phase: To construct an optimal DHI by selecting efficient intervention aspects
- Evaluation Phase: To validate the efficacy of an optimized DHI
- Implementation Phase: To put in place and manage an efficient DHI
Digital Framework of Digital Health Devices
Digital health includes mobile health (mHealth), health information technology (IT), wearable devices, telehealth, telemedicine, and personalized medicine. With the healthcare providers’ rapid transition to virtual care, digital use has increased with time. Overall adoption of telemedicine among the population has reached approx. 80%, making it the go-to method for prescription treatment and minor illnesses. The basic architecture or digital framework of wearable and non-wearable devices is shown below:
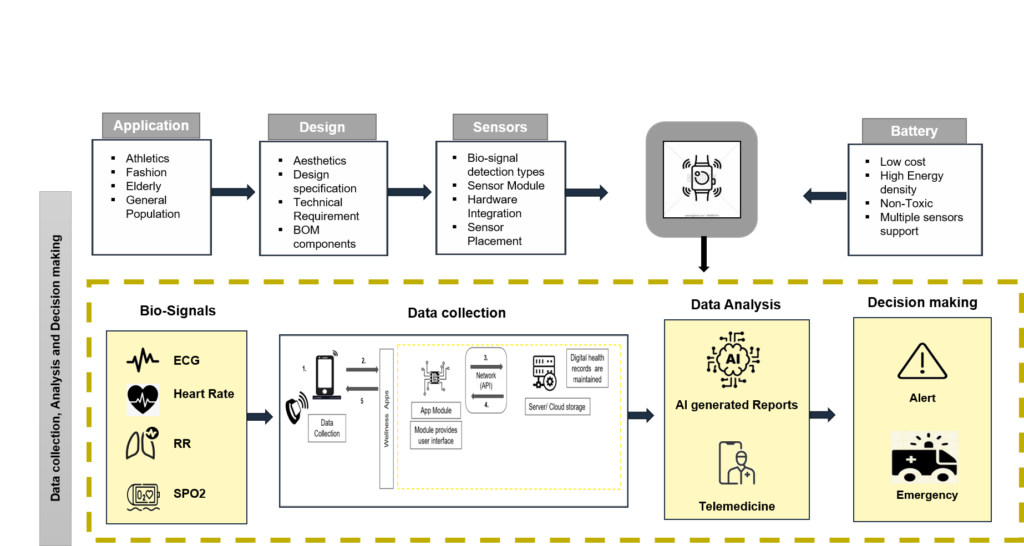
Figure 2: Basic Digital Framework of Wearables and Non-Wearables
The future’s digitally enabled healthcare system holds the key to genuinely integrating people into healthcare systems. It will fundamentally improve the nature and standard of care.
Important Information on Digital Health Devices
- The design and aesthetics are attributed to multiple factors, including the user’s age, target application, and competitors’ design
- The design and aesthetics are attributed to multiple factors, including the user’s age, target application, and competitors’ designs. Wearable devices come in various types, such as glasses, rings, necklaces, armbands, jackets, pants, and shoes. The design of a wearable device depends on the way it is worn. Generating detailed use cases for the device application is better to ensure that the decided design is aligned with generic user requirements.
- Wearable devices should essentially support for multiple sensors to fetch multiple biosignals. These multiple bio-signals can be heart rate, temperature, etc. Biosensors, used in wearables, measure biomarkers digitally. Also, commonly used sensors are PPG and accelerometers that measure heart rate and movement, respectively. The sensing mechanism and algorithms are critical in evaluating any biosignal specific to the sensor.
- Battery life remains one of the most crucial USPs of any digital device. Marketing strategies are centered on extended battery life. Thus, it is ideal for any digital device to use a battery that supports the prolonged working of the device. With the next generation of wearables that might focus on multiple parameters, monitoring along with continuous monitoring of signals will require robust battery solutions.
- Biosignals, or raw data captured from a user, are collected on local hardware or sent via the cloud for further processing. In-house AI-based algorithms can analyze the processed data, and results are displayed instantly. In digital devices with support for teleconsulting, the data is sent to a healthcare provider who analyzes and responds to the patient.
Digital Framework of M-health App
- Designing a digital m-health app involves similar frontend and backend technologies present in a regular app. Differentiation lies in enhanced focus upon encryption, as m-health apps that are FDA-approved for medical use are subject to HIPAA compliancy.
For example, in prescription-based apps, a doctor can ask the patient to wear a portable data-collecting device, which transfers the data via an app; using that personal data requires apps to be HIPAA compliant. Example: ISR (Information Systems Research Framework) is a scientifically validated framework for designing m-health apps. The framework focuses on researcher-practitioner relationships. The researchers here are defined as individuals who initiate the design project, investigate the knowledge associated with the design, and cooperate with the practitioners. The practitioners are the professionals working in the design context.
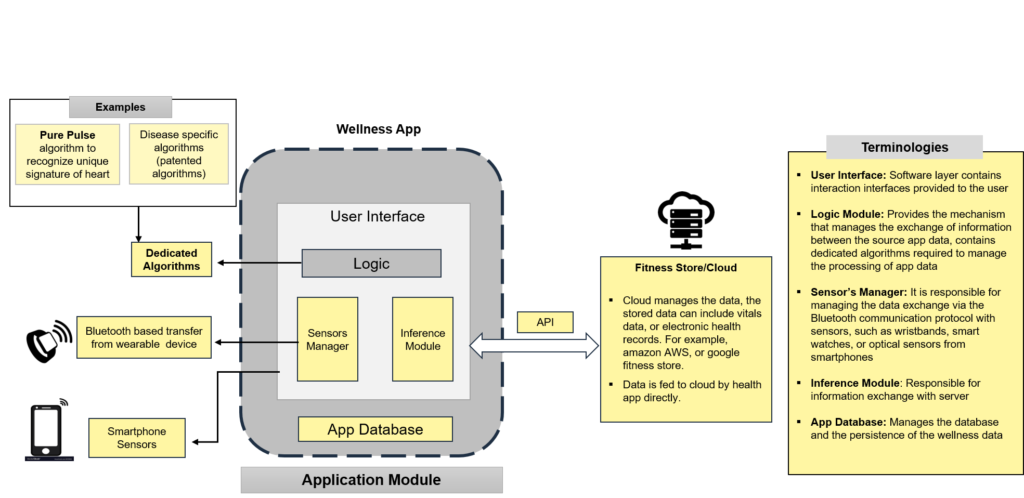
Figure 3: Components of m-health app and digital framework
Factors Driving Faster Technology Adoption
Recent advancements in digital technology during a pandemic have led to the development of many digital healthcare products. Researchers have evaluated a few variables to understand the behavior of consumers that influence the mass adoption of these products.
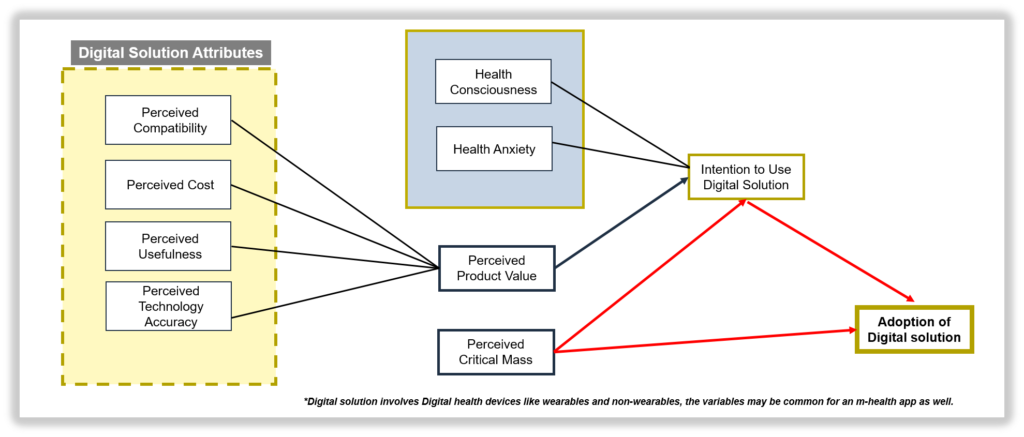
Figure 4: Digital Solutions Attributes
The variables are:
- Perceived Product Value (PPV): The general perception of wearable technologies in the digital health industry is determined by the balance between their advantages and expenses, which ultimately influences their appeal to consumers.
- Perceived Compatability (PCT): Degree of how well a technology can be integrated with existing technologies. Digital devices are highly focused on increasing PCT values.
- Perceived Technology Accuracy (PTA): The precision, accuracy, and legitimacy with which digital devices generate information is known as PTA. FDA-approved digital solutions score higher on PTA.
- Perceived Usefulness (PUS): The extent to which an individual holds the belief that employing a specific system will enhance their overall performance
- Perceived Cost (PCO): The degree to which a person believes that using a digital device would cost money. Higher PCO leads to poor adoption. For premium products, PCO may lead to higher adoption.
- Health Consciousness (HCS): Refers to how well consumers’ health concerns are incorporated. Higher HCS leads to higher adoption
- Health Anxiety (HAY): Highly health-focused individuals who are anxious about their health are generally expected to adopt solutions quickly
- Perceived Critical Mass (PCM): The point at which many consumers have utilized and adopted the technology
Challenges and Future Directions
Wearable or m-health app development suffers from similar fundamental problems, such as ensuring data security and regulatory compliance. Numerous vulnerabilities in mHealth apps might be caused by inadequate security procedures and a deficiency of security expertise on the part of developers. Moreover, as more devices and platforms become available, paying close attention to getting the data right and ensuring users can easily access it is essential.
While challenges exist, overcoming them is vital to building user trust and delivering effective digital health solutions. Integrating generative AI technology to facilitate decision-making is an exciting prospect on the horizon and looks promising. Collaboration, ongoing updates, and resource allocation are key to success while implementing digital health solutions.
Conclusion
With the help of approachable and encouraging healthcare provider teams operating in adaptable, integrated, interoperable, and digitally enabled care environments, digital health connects and empowers individuals and populations to manage their health and wellness. These environments strategically use digital tools, technologies, and services to change the way that healthcare is provided. Understanding the obstacles in developing the digital framework will assist healthcare businesses in overcoming or mitigating the challenges and succeeding in their digital transformation process. Firms must grasp the core building blocks of the digital transformation process and the important areas it touches on, namely customer experience, operational processes, and dynamic business models, to make a smooth transition. Moreover, healthcare organizations must harness the combined power of human ingenuity and technology to increase digital adoption. However, certain gaps exist while developing any strategy, such as;
- Evaluating and validating the digital framework
- Identifying the right manufacturing partners/ suppliers who have expertise in the field
- Use the right go-to-market strategy while addressing the consumer variables parallelly
Addressing these gaps is essential for developing any successful commercial digital health solution.