Cancer vaccines are a potential research-based approach to cancer management and therapy that uses the immune system to target and remove cancer cells. These vaccines attempt to prevent the development of certain malignancies by targeting microorganisms linked to these diseases, such as the HPV vaccine, which is intended to reduce cervical cancer incidence. Furthermore, cancer vaccines can treat existing malignancies by triggering immune responses to specific cancer antigens.
Cancer vaccines are considered for providing alternative types of management that may be more suitable under certain circumstances than traditional techniques of treatment such as surgery, chemotherapy, and radiation therapy, particularly for tumors that are either difficult to treat or relapse often. Cancer vaccines provide a host-directed strategy for changing the course of cancer treatment and care, improving the possibility of improved patient outcomes with fewer side effects as a result of the immune system’s innate specificity for cancer cell destruction. However, more research is needed to assess the potential of treating endometrial cancer, broadening its use to other types of cancer, and addressing issues such as diverse tumor subtypes and anti-tumor immune responses.
Insight into Oncologic Vaccination
Traditional vaccines mainly offer prevention against disease. However, cancer vaccines are for the treatment of existing cancer (in contrast to a preventive vaccine). Irrespective of challenges, including tumor heterogeneity and immune evasion, personalized vaccine strategies, combination therapies, and optimizing delivery methods are being pursued by ongoing research efforts for better efficacy and accessibility. Cancer vaccination is seen as a driving force in the endless search for effective cancer treatments because it might change the way cancer patients are treated.
Classes of Anti-Cancer Vaccines
The cancer vaccines are classified into various types according to their formulation, action mechanism, and clinical applications. These include:
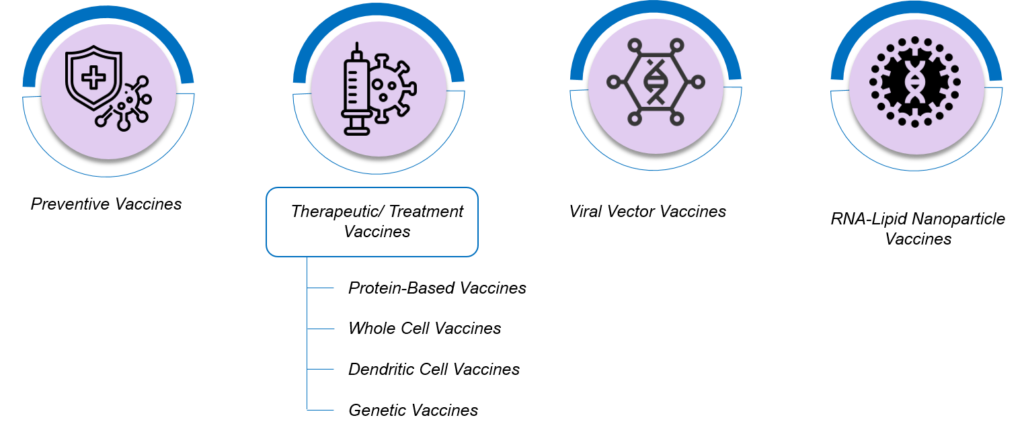
Figure 1: Major Segmentation of Cancer Vaccines
- Preventive Vaccines: These vaccines are formulated to prevent specific cancers by targeting the infectious agents that cause them, such as the HPV vaccine for cervical cancer. These vaccines operate by prompting the immune system to identify and clear the disease-causing organism before a tumor evolves.
- Therapeutic/ Treatment Vaccines: Therapeutic vaccines target patients already diagnosed with tumors/malignancies. The purpose is to modulate the immune system into recognizing and attacking tumor cells, which may lead to the regression of tumors or a prolonged control of illness. Based on their compositions and mode of operation, therapeutic vaccines can be further classified into:
- Peptide or Protein-Based Vaccines: Consists of specific peptides or proteins that are obtained from tumor-specific antigens (TSAs) or tumor-associated antigens (TAAs). These vaccines trigger the immune system to spot and kill malignant cells, indicating these antigens.
- Whole Cell Vaccines: In this kind of immunotherapy, the entire tumor cells or matter derived from these cells are used as an antigen. Through these vaccines, an array of different tumor antigens may be shown to the immune system that might help evoke an immune response all through the tumor area.
- Dendritic Cell Vaccines: Dendritic cells have an important function in beginning immune responses; they are taken from the patient, loaded with tumor antigens, and then introduced into his or her body to activate T cells against the cancer. Dendritic cell vaccines are individualized and focus on tumor antigens that are specific to that particular patient.
- Genetic Vaccines (DNA or RNA Vaccines): The genetic material encoding the tumor antigens instructs the cells to produce the required antigens, resulting in triggering an immune response. Genetic vaccines can activate both humoral and cellular immune responses against cancer.
- Viral Vector Vaccines: Modified viruses introduce tumor antigens into the body and stimulate an immune response through viral vector vaccines. Popular viral vectors in cancer vaccine development comprise poxviruses, lentiviruses, and adenoviruses. These vectors have been modified through genetic engineering so that they are not able to reproduce or cause disease, making them harmless for use as vaccine carriers.
- RNA-Lipid Nanoparticle Vaccines: These innovative vaccine platforms involve the delivery of tumor antigens encoded by mRNA into cells for their expression in the host. These vaccines have shown great potential in preclinical and early clinical trials for diverse types of cancers.
Advancements and Clinical Trials/ Studies
However, it is a fact that the development and clinical transfer of cancer vaccines have faced significant challenges. Nonetheless, notable progress has been made in the field recently, as several cancer vaccines have successfully gone through preclinical investigations and clinical trials.
For instance, therapeutic cancer vaccines targeting prostate cancer (Provenge) and melanoma (Yervoy) are among the most well-known. These vaccines have proven their efficiency in extending the lives of patients suffering from the late stages of these conditions, hence confirming the idea of using immunotherapy for treating malignant neoplasms.
Furthermore, ongoing efforts are to optimize vaccine design, explore new targets for antigens, and devise combination approaches with other immune therapy modalities to potentiate their efficacy. For encouraging early results from personalized cancer vaccine trials – such as those on glioblastoma and melanoma – indicative of the possibility of prolonging patient survival.
Challenges in Cancer Vaccine Development
Despite advances, there are still many remaining challenges. Their effective development and use call for an interdisciplinary approach, with immunology, oncology, genetics, bioinformatics, and vaccine technology at the forefront. Some of these include:

Figure 2: Challenges in Cancer Vaccine Development
Cancer Heterogeneity/ Personalization: Genetic and phenotypic variation typically in cancer cells within a tumor makes it difficult to find universal antigen targets that can be used for vaccine development.
Immune Suppression: The tumor micro-environment has different mechanisms by which tumor cells escape immune surveillance, including immune response suppression. Immune suppression needs to be overcome to enable the effectiveness of cancer vaccines.
Immune Evasion Mechanisms: Cancer cells have developed several ploys to avoid immune responses that detect them, which are resistant to their destruction. The anti-tumor immune response in cancer vaccines has to be powerful enough to overcome these immune evasion ploys.
Optimal Antigen Selection: Appropriate selection of tumor antigens that can produce immune responses differentially in cancer cells and are suitable for vaccine-induced antitumor effects. However, the selection of antigens is complicated and still a dynamic process.
Logistical Barriers: Complicated manufacturing processes are required for personalized cancer vaccines and may not be possible due to logistic implications and financial constraints on their wide use.
Future Directions and Opportunities
To create cancer vaccines and improve results in cancer patients, advanced immunomodulatory agents, accelerated screening techniques, and next-generation sequencing paved the way for a bright future. Quite a few exciting areas have the potential to significantly advance cancer immunotherapy and improve patient outcomes when exploring future directions and opportunities for cancer vaccines. A few main areas to focus on include:
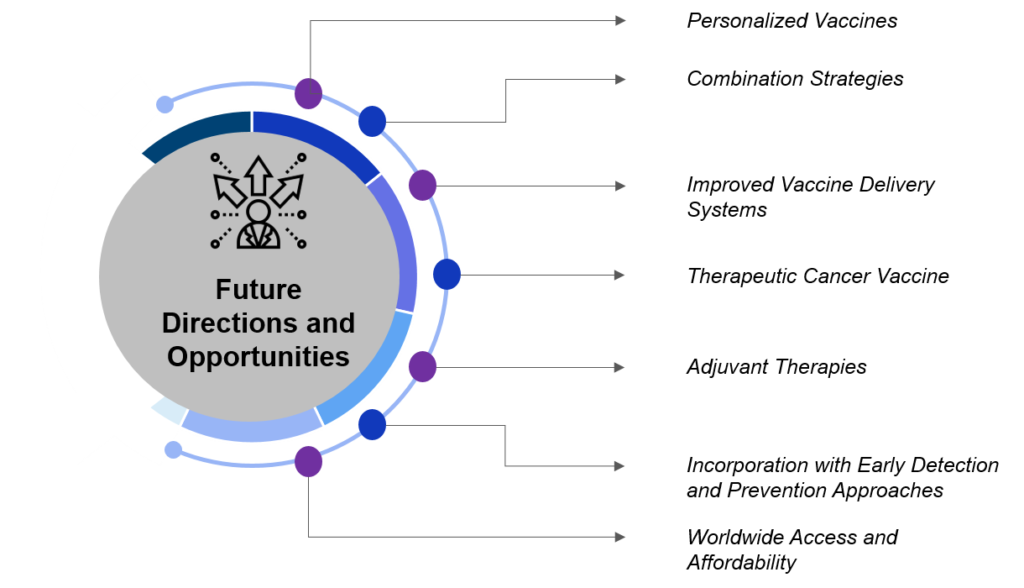
Figure 3: Future Directions and Opportunities
- Personalized Vaccines: Also known as neoantigen vaccines, are made for an individual’s genetic mutations. These vaccines aim to develop highly targeted immunity responses toward cancer by focusing on neoantigens that are not present in healthy cells. Clinical examination of customized cancer vaccines in patients with advanced cancers has shown promising outcomes, highlighting this approach’s feasibility and therapeutic potential.
- Combination Strategies: Optimizing the combination of cancer vaccines and other immunotherapies, such as checkpoint inhibitors or adoptive cell therapy, indicates a promising future for enhancing antitumor immune responses and overcoming resistance mechanisms.
- Therapeutic Cancer Vaccine: The main aim of therapeutic cancer vaccines is to control cancers by stimulating the immune system to recognize and attack tumor cells. Subsequent developments in this segment would be in the formulation of vaccines, identification of different tumoral companion proteins, and improvement of vaccination schedules for better medical efficiency.
- Adjuvant Therapies: Scientists continuously seek novel adjuvants to enhance cancer vaccine efficacy by helping the immune system identify tumor antigens. Adjuvants are known to increase the immune response to vaccines. Also, modify the tumor’s microenvironment to make it more conducive to immune-mediated destruction.
- Incorporation with Early Detection and Prevention Approaches: Combining cancer vaccines with early diagnostic approaches may contribute to more efficient therapy, thereby increasing the chances of survival.
- Worldwide Access and Affordability: Enhancing vaccine stabilization to enhance vaccine deployment in various healthcare settings and design and development of low-cost methods of vaccine manufacturing.
Potential Players Shaping the Domain/ Market of Cancer Vaccines
The domain of cancer vaccines is quickly changing and is driven by contributions from pharmaceutical companies, biotech organizations, universities, and research institutions. These players are utilizing diverse technologies and approaches, from mRNA and DNA-based vaccines to personalized and cell-based immunotherapies, to improve and develop cancer vaccines. Their collaborative efforts are transforming the future of the entire oncology domain, focusing on making better patient outcomes through new strategies in immune therapy. Here are some notable players, including GSK, that are engaged in developing cancer vaccines.

Figure 4: Key Players Actively Working in Cancer Vaccine Development
Conclusion
In conclusion, cancer vaccine development marks an important step forward in cancer therapeutics, which uses the body’s natural immune response to target and eliminate cancer cells. Recent advancements in personalized vaccines, combination therapies, cancer therapy, and delivery systems address tumor heterogeneity and immune evasion challenges, showing significant potential. Continuous research and innovation bring hope for the future of cancer immunization and for improving vaccine efficacy, accessibility, and patient outcomes. Making this novel cancer care transformation successful will need a combined effort by researchers, health professionals, and stakeholders to surmount current challenges and translate these breakthroughs into patients worldwide.