Breaking Barriers in Respiratory Care: The Tech-Driven Future of Lung Health
Over the years, respiratory care has changed dramatically, whereby technology, treatment methods, and accessibility to patients have revolutionized the management of respiratory illness. Indeed, the phenomenal changes occurring in the field of respiratory care are characterized by the application of artificial intelligence (AI), smart wearables, the Internet of Things (IoT), and advanced drug delivery systems. These advancements include early detection of diseases, real-time monitoring, and personalized treatment for asthma and other lung disorders such as chronic obstructive pulmonary disease (COPD) and sleep apnea. It has improved the quality of care and patient experience, but the barriers to offering the best care still stand.
Breaking these barriers will truly impact patient outcomes and ensure equitable access to respiratory health care in our diverse populations. This article will discuss the significant breakthroughs that will enable practitioners to break down barriers to respiratory care, with the ultimate aim of restoring the lives of their patients across the world.
Technologies that are Transforming Respiratory Care
Emerging technologies are improving the management and treatment of respiratory conditions, which enhances the quality of life (QoL) for patients with chronic lung diseases, such as asthma, COPD, cystic fibrosis, etc., while also improving patient outcomes. Here are some key technologies transforming respiratory care:
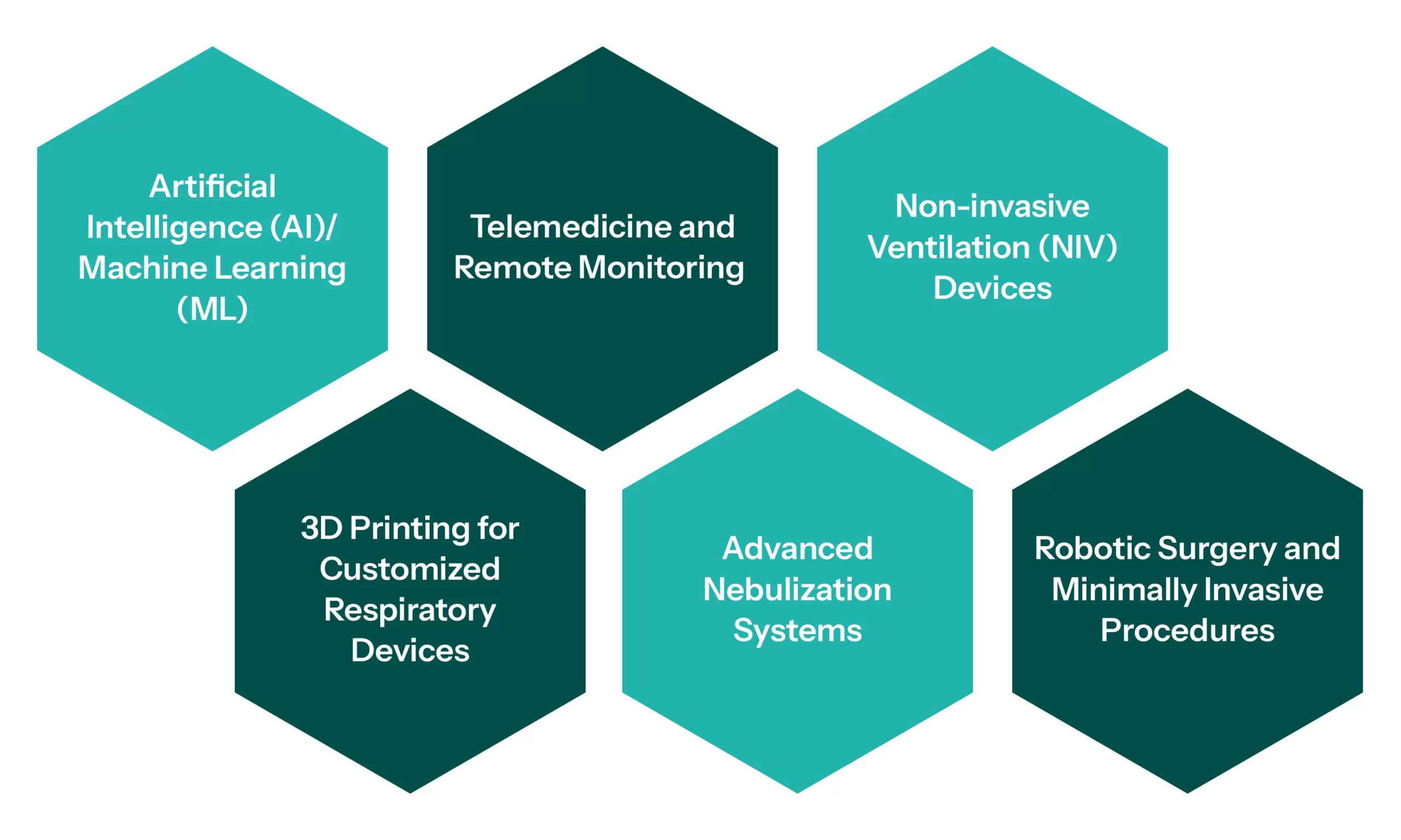
Artificial Intelligence (AI)/ Machine Learning (ML)
AI-driven tools for diagnostics are transforming respiratory care by enabling faster and more precise detection of conditions such as COPD, asthma, lung cancer, etc. With the help of ML algorithms, lung function tests, radiographic images, and patient history can be used to assist health professionals in making their decisions. AI/ ML allows clinicians to make the right decisions in complex cases by mining huge volumes of patient data to provide recommendations. These also help derive a personalized treatment plan for the patient, depending on the patient’s history, genetics, and real-time data.
To explore broader applications of AI in healthcare, discover our insights on AI-powered Predictive Maintenance
Telemedicine and Remote Monitoring
Devices monitoring respiratory functions, such as pulse oximeters and spirometers, can now sync with smartphones/ smart-devices for remote lung function tracking. This permits more frequent and continual assessment of the conditions. Respiratory patients can consult with their healthcare providers remotely, thereby relieving the frequency of visits to the hospital for those who have chronic disorders/ conditions. Remote monitoring systems allow healthcare personnel to track respiratory health remotely, thus facilitating easier management of patients with chronic disorders. For example, alerting patients to deteriorating conditions, taken as continuous monitoring of patient oxygen levels or peak flow, can allow additional medical intervention.
Non-invasive Ventilation (NIV) Devices
Advances in portable NIV equipment allow patients with respiratory failure to be treated outside the hospital, improving mobility and quality of life (QoL). Technologies that automatically adjust pressure settings based on the patient’s breathing patterns improve comfort and treatment efficacy.
To understand how non-invasive technologies are reshaping all medical treatments, read our article on Non-invasive Treatments Revolutionizing Cancer Care
3D Printing for Customized Respiratory Devices
3-Dimensional printing permits the creation of tailored respiratory devices such as inhalers, mouthpieces, face masks, etc. This would help improve comfort and effectiveness for patients with specific anatomical or functional needs. For instance, 3D-printed lung models based on patient-specific CT scans are being used for pre-surgical planning, training healthcare providers, and educating patients about their conditions.
Advanced Nebulization Systems
Mesh nebulizers employ ultrasonic or vibrating mesh technology to create smaller and more uniform aerosol particles, aiding more efficient medication delivery as opposed to traditional nebulizers. Advanced nebulizers are equipped with smart technology such as Bluetooth connectivity to monitor usage and provide reminders for medication adherence. Smart inhalers track when and how often patients take their medications, so they provide real-time data to both the patient and their health care provider.
Robotic Surgery and Minimally Invasive Procedures
Robot-aided bronchoscopy makes much more precise navigation within the lungs, improving the ability to biopsy and treat diseases affecting the lungs with minimal invasiveness. An example is the new methods for severe emphysema that are now minimally invasive; they allow the excision of spoiled lung tissue and shorter recovery periods with fewer complications.
To discover more about cutting-edge robotic surgical innovations, explore our insight into robotic surgery advancements
Challenges in Accessibility
Technological advancements have made great strides in improving the management of respiratory disease, yet several access issues remain to achieve the same. Such access deficiencies are always taken as huge impediments to fulfilling the right and warranting a timely setting of health and comfort for a patient. Here are some of the key issues in accessibility to respiratory care:

Geographic Barriers:
Patients living in various rural areas or hard-to-reach locations might limit or restrict their access to respiratory care professionals, diagnostic tests, and treatment facilities. Traveling long distances to urban centers would not only incur unreasonable costs for those suffering from chronic respiratory ailments but also take a significant amount of time and, in many cases, would become physically demanding for the patient. Furthermore, many hospitals or clinics might not have the facility of advanced respiratory care technologies, such as ventilators, nebulizers, or imaging tools, which is another limitation to providing optimal care and management to the patients.
Economic and Insurance Barriers:
Respiratory treatments, including medications, inhalers, nebulizers, and oxygen therapy, can be prohibitively expensive for some patients. Most people often can’t afford such important treatments, medications, or even doctors’ visits without proper health insurance coverage. Some respiratory treatments would be covered by insurance; however, most advanced therapies, like home oxygen therapy or some new drugs for diseases such as COPD, asthma, etc., might have a gap in the coverage. This would, therefore, deny the patients who need them most access to treatment.
Limited Access to Specialized Care:
There is a shortage of qualified pulmonary practitioners, particularly in underserved regions. This has created incredible difficulties for patients and complicated many advanced respiratory illnesses such as chronic obstructive pulmonary disease (COPD), cystic fibrosis, pulmonary fibrosis, and so on, even in patients with an established diagnosis. Even when specialists are available, some of the medical providers, mostly general practitioners, do not have the training or experience to handle advanced respiratory conditions adequately, which can lead to delays in diagnosis or suboptimal treatment.
Technological Barriers:
While advanced diagnostic tools, smart inhalers, and telemedicine substantially improve patient care, not all patients and healthcare facilities can access the technology. Hospitals or clinics in low-income or rural areas may not have the available resources to buy modern equipment. Telehealth options and remote monitoring devices can be problematic to integrate for patients who are not proficient in the digital world or those without access to a reliable internet connection. In particular, many older adults experience difficulty with smartphone apps or other technology platforms.
Limited Rehabilitation Services:
Pulmonary rehabilitation, which is crucial for patients with chronic respiratory diseases like COPD, is often underutilized. Limited referral sources for pulmonary rehabilitation programs, especially in smaller towns or rural areas, lead to many patients missing opportunities to improve lung function, exercise tolerance, and quality of life (QoL). Many patients need adjunct support services like smoking cessation programs, mental health counseling, and nutritional counseling in addition to rehabilitation. These types of services may not always be available or beneficial for certain patients.
Solutions and Moving Forward
Efforts are being made to address these barriers/ challenges, but evolution is still needed. Some potential solutions include:
- Expanding telehealth and remote monitoring to reach underserved areas
- Increasing the availability of financial assistance and health insurance coverage for advanced and qualitative respiratory care
- Providing education and training on inhaler use and disease management for both patients and healthcare providers
- Improving health literacy through community outreach programs and multilingual resources
- Developing policies and initiatives to reduce air pollution and improve environmental factors that contribute to respiratory disease
- Expanding access to affordable treatment
While respiratory care has advanced significantly, accessibility remains a major challenge that requires coordinated efforts from governments, healthcare providers, and communities to ensure equitable care for all patients.
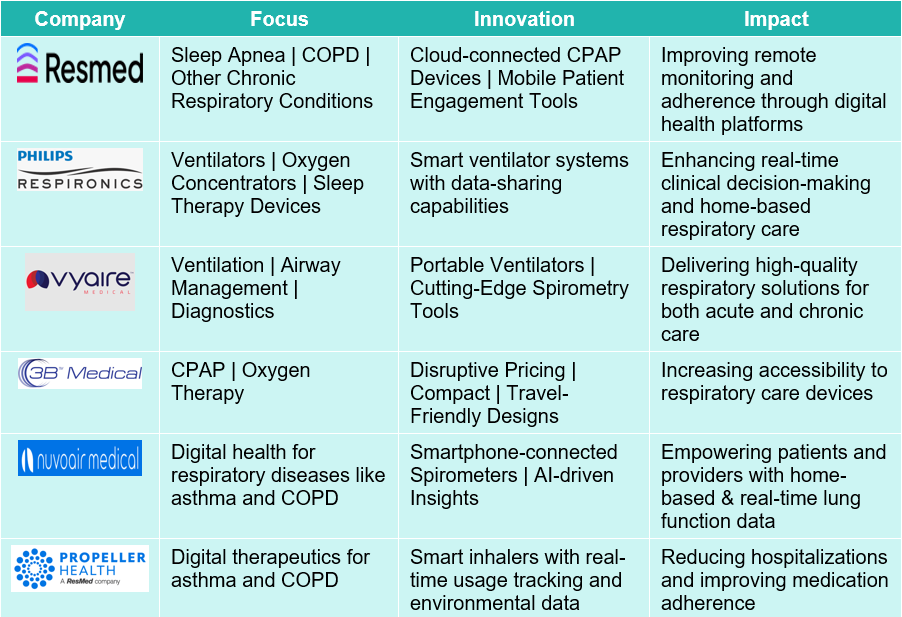
Primary Contributors to Breaking Barriers in Respiratory Care

Companies that are Breaking Barriers in Respiratory Care
Conclusion
Breaking barriers in respiratory care encompasses a comprehensive approach that combines developments in technology, upgraded access to care, superior education, and boosted support for underserved populations. By leveraging telemedicine, remote monitoring, patient education, and culturally competent care, we can enhance the quality of life (QoL) for patients with respiratory illnesses.
In addition, policies must be modified, community partnerships developed, and social determinants of health must become paramount considerations to ensure fair access to care for every individual, no matter the person’s background or resources. Ultimately, by breaking barriers, there will also be better management, outcomes, and quality of life (QoL) for patients with various respiratory conditions.